All published articles of this journal are available on ScienceDirect.
Severe Lower Limb Edema Complicating COVID-19 in a Rheumatoid Arthritis Patient: A Case Report
Abstract
Background
COVID-19 is primarily associated with acute respiratory symptoms but can also cause non-respiratory complications, such as lower limb edema. The mechanisms behind this remain unclear, posing diagnostic challenges for clinicians.
Case Presentation
A 73-year-old woman with rheumatoid arthritis developed severe lower limb edema following COVID-19. The edema, attributed to systemic inflammation and hypoalbuminemia, was successfully treated with corticosteroids and diuretics.
Conclusion
This case highlights the importance of a thorough differential diagnosis of lower limb edema post-COVID-19. After excluding thrombosis and lymphedema, we concluded that systemic inflammation and hypoalbuminemia were the primary contributors. Thus, early recognition and targeted treatment are crucial for managing such cases.
1. INTRODUCTION
Since its declaration in March 2020, the Coronavirus Disease 2019 (COVID-19) pandemic has led to extensive reports documenting the diverse symptoms and complications of SARS-CoV-2. The virus not only causes acute respiratory syndrome but also significantly affects critical organs like the brain, heart, and liver, with non-respiratory symptoms being even more prevalent [1]. Many aspects of COVID-19 remain unclear, including lower extremity edema, which has been reported after infection or mRNA vaccination. Potential causes include thrombosis related to COVID-19-induced inflammation, hypoxia, immobilization, increased intravascular coagulability, and increased lymphatic permeability [2, 3]. In some patients, preexisting lymphedema may worsen with cellulitis after COVID-19 mRNA vaccinations [4]. Here, we present a patient with rheumatoid arthritis who developed severe lower limb edema post-COVID-19 infection.
2. CASE REPORT
A 73-year-old woman with seropositive rheumatoid arthritis in clinical remission attended a routine follow-up on April 17, 2024. Her medications included methotrexate, folic acid, leflunomide, rebamipide, calcium/cholecalci ferol, and ferrous sulfate. She was also on telmisartan/amlodipine/hydrochlorothiazide for hypertension and rosuvastatin for dyslipidemia, with a history of bilateral knee replacements in 2021. A month after contracting COVID-19, she developed acute bilateral lower limb edema with severe swelling, pain, and mobility impairment, significantly impacting her daily life. Examination revealed symmetrical pitting edema from the waist to the feet (Fig. 1A, B). Her rheumatoid arthritis remained well controlled, with no prior similar symptoms or recent medication changes. The patient received multiple COVID-19 vaccinations without adverse effects: AstraZeneca (AZD1222) in early 2021 (first and second doses), Moderna (mRNA-1273) in January 2022 (third dose), Pfizer (BNT162b2) in June 2022 (fourth dose), Pfizer BA.4/5 in December 2022, and Pfizer XBB.1.5 during the 2022–2023 winter season. She contracted COVID-19 for the first time in March 2024, presenting with fever, cough, and fatigue. After testing positive at a local hospital, she was treated symptomatically with chlorpheniramine, pelargonium sidoides, and mosapride but did not receive antiviral therapy. While her respiratory symptoms resolved within days, she developed acute lower limb edema with severe pain shortly after. Initial treatment with oral amoxicillin/clavulanate, bromelain, and loxoprofen for three days was ineffective, leading her to visit our clinic for further evaluation.
The patient’s vital signs were stable. Laboratory tests showed leukocytosis (WBC 14,120/mm3), mild anemia (Hb 10.9 g/dL), hypoalbuminemia (3.08 g/dL), and elevated CRP (4.8 mg/dL), with normal platelet count, ESR, creatinine, and urinalysis. Coagulation markers (D-dimer, FDP), anti-phospholipid antibodies, and complement levels were within normal limits. Echocardiography and renal function tests showed no abnormalities. CT venography ruled out deep vein thrombosis (DVT), and contrast-enhanced CT scans of the chest, abdomen, and pelvis revealed no significant pathology. Lymphoscintigraphy confirmed normal lymphatic drainage, ruling out lymphedema (Fig. 2A-C). Despite the absence of fever, elevated CRP prompted empirical IV ampicillin/sulbactam. After three days without improvement, oral prednisolone (10 mg bid) and furosemide (20 mg bid) were added, leading to rapid symptom relief. The patient reported significant improvement, emphasizing the importance of timely diagnosis and treatment. Blood cultures were negative. The patient was discharged on oral amoxicillin/clavulanate, furosemide (40 mg bid), and prednisolone (15 mg qd). At the one-week follow-up, edema had significantly improved, with only mild, intermittent swelling (Fig. 1B), and CRP and albumin levels normalized, allowing discontinuation of all medications. By four weeks, the edema had fully resolved, with no recurrence at the six-month follow-up. Comprehensive evaluations ruled out anatomical abnormalities, thrombosis, and lymphedema, confirming a favorable prognosis with complete symptom resolution.

Gross appearance of lower legs. (A) Initially, extensive lower leg edema was observed. (B) At follow-up 1 week after discharge, substantial improvement in edema was noted. At follow-up 5 weeks after discharge, edema was absent.
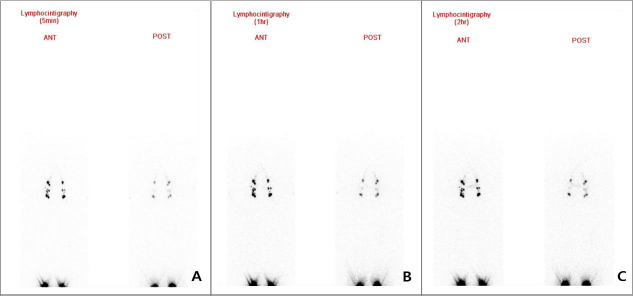
Lymphoscintigraphy images at 5 minutes (A), 1 hour (B), and 2 hours (C) after radiotracer injection. Both anterior (ANT) and posterior (POST) views are shown. There is symmetric and normal tracer uptake and progression over time, with no evidence of dermal backflow or delayed transit. These findings indicate normal lymphatic drainage and no signs of lymphatic obstruction or leakage.
3. DISCUSSION
In May 2023, the World Health Organization (WHO) lifted the Public Health Emergency of International Concern (PHEIC) for COVID-19. However, its clinical manifestations and mechanisms remain unclear, and sporadic endemic infections persist. Lower extremity or generalized edema has been reported post-COVID-19 or after mRNA vaccination, with some cases linked to thrombosis or lymphedema. Studies have noted vascular abnormalities in cases with skin lesions [2, 3, 5-7]. Besides traditional thrombotic risk factors like ICU immobilization and high Padua scores, COVID-19 itself exhibits prothrombotic properties, increasing thrombosis and pulmonary embolism rates. Additionally, post-vaccination lymphedema and cellulitis have been documented [4,8,9], with lymphoscintigraphy playing a key role in aiding diagnosis. Skin biopsies in affected patients revealed serum and erythrocyte extravasation in the dermis and epidermis [7, 10].
This report describes a case of acute lower extremity pitting edema following COVID-19 in a patient with rheumatoid arthritis, hypertension, hyperlipidemia, and prior bilateral knee arthroplasty. Diagnosing the underlying cause was challenging due to overlapping etiologies, including deep vein thrombosis (DVT), lymphedema, intraabdominal pathology, cardiac and renal dysfunction, and systemic inflammation. Extensive workup ruled out DVT (CT venography), cardiac and renal dysfunction (echocardiography, renal tests), and lymphedema (lymphoscintigraphy). Despite normal imaging, hypoalbuminemia and elevated CRP suggested systemic inflammation as the primary mechanism. No evidence linked the patient’s rheumatoid arthritis, hypertension, hyperlipidemia, or medications to the sudden onset of bilateral lower limb edema, making COVID-19 the most likely cause. She had no prior edema despite long-term amlodipine use, stable disease, and no recent medication changes. Elevated inflammatory markers were also unexplained by her chronic conditions or medications, reinforcing a temporal and causal link between COVID-19 and acute edema. The edema was likely driven by hypoalbuminemia from systemic viral infection, with elevated CRP reflecting inflammation. This case highlights the importance of ruling out thrombosis and lymphedema in post-COVID-19 patients. However, a limitation is the inability to determine whether steroids or diuretics played a greater role in symptom resolution, although diuretics likely had the most significant effect.
CONCLUSION
This case highlights the diagnostic complexity of new-onset lower extremity edema following COVID-19, particularly in patients with underlying autoimmune and cardiovascular comorbidities. While the symptoms of the patient resolved with corticosteroids and diuretics, the temporal association with COVID-19 and the exclusion of other common causes suggest that systemic inflammation and hypoalbuminemia may have contributed to the condition. It may be helpful for clinicians to be aware of the potential for such post-infectious complications in patients with similar presentations. Further research is warranted to clarify the underlying mechanisms and to guide appropriate management strategies.
AUTHORS’ CONTRIBUTIONS
K.M., K.S.H.: Conceptualisation; K.M., K.S.H.: Data curation; K.M., K.S.H.: Original draft: J.C.I., K.S.H.: Writing – review & editing.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| DVT | = deep vein thrombosis |
| WHO | = World Health Organization |
| PHEIC | = Public Health Emergency of International Concern |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Institutional Review Board of Konyang University Hospital, Republic of Korea (KYUH 2024-05-16).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
ACKNOWLEDGEMENTS
Declared none.