All published articles of this journal are available on ScienceDirect.
Nail Involvement in Cutaneous Psoriasis or Psoriatic Arthritis: Ultrasound and Microscopic Correlation
Abstract
Introduction
Onychodystrophy is common in individuals with psoriasis and psoriatic arthritis and is frequently associated with disease severity.
Objective
The objective of this study is to correlate ultrasound findings with alterations in nail clippings from patients with psoriasis and psoriatic arthritis, with and without nail dystrophy.
Method
Transversal study involving 120 patients distributed into four groups (psoriasis with and without onychodystrophy, psoriatic arthritis with and without onychodystrophy). All patients underwent clinical, ultrasound and microscopic evaluations of the nails.
Results
Neither ultrasound nor nail clipping results alone were able to consistently differentiate patients with and without arthritis. Nail clipping evaluation showed greater nail plate thickness in patients with onychodystrophy (p=0.006). The presence of neutrophils was correlated with higher values for affected body surface area (p=0.0032) and PASI (p=0.0032) and NAPSI (p=0.008) scores, indicating a link between psoriasis severity and inflammation. Significant correlations were found between ultrasound and microscopic variables related to the nail plate: microscopic thickness was correlated with grayscale Doppler findings (p=0.002) and nail bed thickness was measured by ultrasound (p=0.012). The presence of neutrophils was associated with increased nail bed thickness (p=0.005) and grayscale findings in the nail plate (p=0.00001). For the first time, microscopic blurring of the nail transition zone was linked to greater thickness of the nail bed measured by ultrasound (p=0.001) and increased color Doppler activity (p=0.018).
Conclusion
This is the first investigation correlating microscopic and ultrasound alterations in the nails of individuals with psoriasis and psoriatic arthritis, contributing to better comprehension of the markers of severity and inflammation.
1. INTRODUCTION
Onychodystrophy is a common condition in individuals with psoriasis, occurring in about 56% of cases of psoriasis vulgaris [1] and in approximately 80% to 90% of those with psoriatic arthritis [2]. Nail clipping (removal of the distal portion of the nail for microscopic analysis) and ultrasound are supplementary tests frequently used to study psoriatic nails and psoriatic arthritis. However, to date, these studies have investigated these methods in isolation. As a result, there are no clear estimates of the sensitivity and specificity of nail ultrasound in comparison with microscopic nail analysis in patients with psoriasis and/or psoriatic arthritis [3-8].
The primary objective of this study was to compare ultrasound and microscopy findings in patients with psoriasis and psoriatic arthritis, both with and without onychodystrophy. This is the first detailed study to correlate microscopic ungual alterations with nail ultrasound.
2. MATERIALS AND METHODS
This transversal study included patients over 18 years of age with psoriasis and psoriatic arthritis, as defined by the CASPAR criteria [9]. Participants were recruited consecutively from an outpatient dermatology clinic at our teaching hospital from November 2020 to January 2022. Patients were excluded if they did not provide informed consent, had positive results for fungi in direct mycological exams or nail cultures, or had a history of nail trauma in the preceding period of 6 weeks, local corticosteroid injections in the distal interphalangeal joints (DIP), or diagnosed osteoarthritis in the hands. The study was conducted in accordance with the Declaration of Helsinki and local regulations, with approval by the hospital ethics committee (process 4.279.067) and written informed consent obtained from all participants.
Patients diagnosed with psoriasis and psoriatic arthritis were evaluated in terms of age, sex, clinical presentation of psoriasis/psoriatic arthritis, presence of nail abnormalities, Psoriasis Area and Severity Index (PASI) score, and Nail Psoriasis Severity Index (NAPSI) score in cases with onychodystrophy, and their epidemiological profiles.
The cohort was divided into four groups: Group 1 – patients with psoriasis vulgaris and clinically normal nails (Pso Normal); Group 2 – patients with psoriasis vulgaris and onychodystrophy (Pso Dystrophy); Group 3 – patients with psoriatic arthritis and clinically normal nails (Arthritis Normal); and Group 4 – patients with psoriatic arthritis and onychodystrophy (Arthritis Dystrophy).
All participants in Groups 1 to 4 underwent comprehensive dermatological and rheumatological assessments. Ultrasound and microscopic examinations were performed on the following nails: for Groups 1 (Pso Normal) and 3 (Arthritis Normal), both the right and left ring (fourth) fingers; for Groups 2 (Pso Dystrophy) and 4 (Arthritis Dystrophy), the most dystrophic nail on each hand (left and right), with two nails per individual, as determined by the NAPSI index.
2.1. Ultrasound Examination
Ultrasound examinations were performed by the same examiner, who was blinded to the clinical data. A high-resolution ultrasound device (MyLab40, Esaote SpA, Genoa, Italy) was used in B-mode or grayscale (GS), power Doppler (PD), and spectral Doppler, with a linear transducer capable of up to 18 MHz. Each patient was evaluated in a climate-controlled room (approximately 24°C) with dim lighting, positioned across from the examiner on an exam bed, with their hands placed in a relaxed position. Patients were instructed not to discuss their clinical condition with the examiner. The examiner evaluated the dorsal appearance of the distal interphalangeal (DIP) joints of the nails where clippings were taken in groups 2 (Pso Dystrophy) and 4 (Arthritis Dystrophy), and the right and left ring fingers in groups 1 (Pso Normal) and 3 (Arthritis Normal). The thickness of the nail bed was measured longitudinally at the eponychium, tracing a straight line between the ventral nail plate and the periosteum. The reference value considered normal was 2 mm or less [10, 11].
The following semiquantitative scale was adopted to analyze the nail plate: GS0: trilaminar structure preserved; GS1: slight alteration in the trilaminar structure or presence of a bend or gap in the nail; GS2: intense alteration in the trilaminar structure, but some segment of the nail still preserved, with more than one bend or gap in the nail; GS3: total loss of the trilaminar structure, thickening, deformity, or loss of the entire nail format or gaps with destruction of the entire nail segment. Findings classified as GS1, GS2 or GS3 were considered abnormal.
The nail bed was analyzed in PD mode to quantify blood flow, using a 15 MHz linear transducer, pulse-repetition frequency of 0.7, and low wall filter. The analyses were conducted in the longitudinal and transversal planes, applying the following semiquantitative scale: PD0: lack of PD signal anywhere in the nail bed; PD1: presence at one point or up to 25% of PD signal anywhere on the nail bed; PD2: presence of two or three isolated points or 25-50% of PD signal anywhere on the nail bed, particularly at the nail insertion; PD3: presence of over 50% of PD signal throughout the nail bed, particularly at the nail insertion. Spectral Doppler measurement was taken where the PD signal was strongest, with the resistance index calculated automatically by the ultrasound device according to the following formula: systolic peak – diastolic flow / systolic flow. A resistance index below 1 indicates inflammation [10, 11]. Only the PD2 and PD3 classifications were considered altered, with PD1 considered normal due to physiological vascularization.
2.2. Nail Clipping
Nail samples were collected by cutting the distal portion of the nail plate measuring at least 5 mm by 2 mm [12, 13]. Samples underwent technical processing for microscopic study, as described previously [14, 15]. The following microscopic parameters were evaluated: the thickness of the nail plate and subungual region (measured in millimeters), and the presence or absence of parakeratosis (corneocyte nuclei in the subungual region), and presence of neutrophils, serous lakes, blood, fungi, and clear/well-defined or blurry ungual transition zone. Microscopic examination was done in a blind manner, without knowledge of which group the sample belonged to.
2.3. Statistical Analysis
Data distribution was assessed using the Shapiro-Wilk test. Descriptive statistics (median, minimum, and maximum) were used to summarize the results for quantitative variables, while categorical variables were expressed as absolute and relative frequencies. For comparisons between groups, the Mann-Whitney and Kruskal-Wallis tests were applied for quantitative variables and Pearson's chi-squared test for categorical variables. The correlation was analyzed using Spearman's rank correlation coefficient. Analyses were conducted in Statistica Statsoft software version 7.0, with p<0.05 considered statistically significant.
3. RESULTS
A total of 120 patients (30 in each group) participated in the study; 46% of participants were female, without significant disparities between the groups. Mean age for all groups was 51.6 years, with no statistically significant differences.
The mean overall PASI score was 4.32; mean PASI score was lower in groups 3 and 4 (Arthritis Normal and Arthritis Dystrophy, respectively, mean=3.42) than the patients with psoriasis in groups 1 and 2 (Pso Normal and Pso Dystrophy, respectively, mean=5.23), a statistically significant difference (p=0.008). This disparity was also seen in for body surface area (BSA): patients with psoriatic arthritis had lower values (2.55) than the group without arthritis (3.75), with statistical significance (p=0.005). As for nail psoriasis severity (as measured by the NAPSI), no significant differences were seen between groups 2 and 4, which presented nail dystrophy (p=0.12). Patients with onychodystrophy exhibited similar scores for PASI (p=0.66) and BSA (p=0.52), regardless of the presence of arthritis.
3.1. Ultrasound Findings
A total of 240 nails (two fingers from each patient in each group consisting of 30 patients) were analyzed. The ultrasound findings revealed that the grayscale findings for the nail plate (Fig. 1) were similar in groups 1 and 3 (psoriasis or arthritic psoriasis without nail dystrophy), while groups 2 and 4 (patients with nail dystrophy) also exhibited similarities.
The results for Power Doppler also showed similarities between groups 3 and 4 (psoriatic arthritis) and groups 1 and 2 (psoriasis). In Power Doppler, no significant differences were observed between cutaneous psoriasis and psoriatic arthritis in patients with onychodystrophy (p=0.16) (Fig. 2). In general, psoriasis and psoriatic arthritis did not exhibit significant differences in the grayscale nail plate findings (p=0.442), Power Doppler nail bed results (p=0.124), or the resistive index (RI) (p=0.758).
3.2. Findings from Nail Clipping Analysis
A total of 240 nails were analyzed, two from each participant in the groups of 30 patients. In the microscopic assessment, the nail plate was thicker in groups 2 and 4 (with dystrophic nails) than in groups 1 and 3 (p=0.006). Significant differences were not observed between groups 2 (Pso Dystrophy) and 4 (Arthritis Dystrophy) with regard to the presence of neutrophils, serous lakes, parakeratosis, blurring of the ungual transition zone (Figs. 3 and 4) or width of the ungual or subungual plate (Table 1). In the correlation between the microscopic alterations and the clinical variables, only the presence of neutrophils was significantly related to higher mean BSA (p=0.032), PASI (p=0.032), and NAPSI (p=0.008) values.
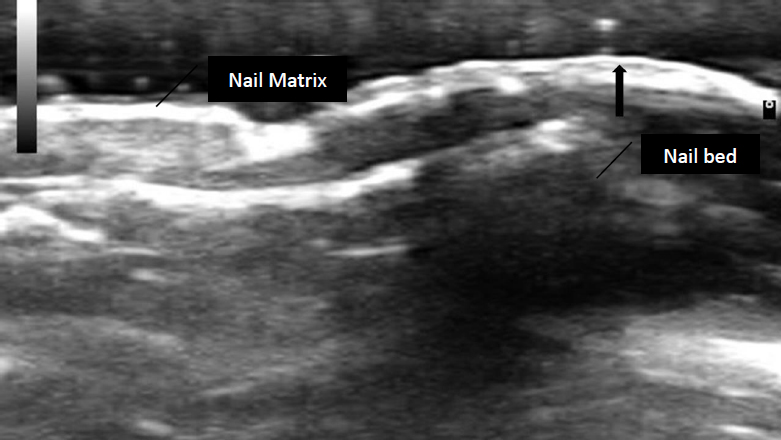
Grayscale ultrasound of the nail in a patient from group 2. Arrow: hyperechoic layer losing normal trilaminar appearance. Image in B-mode, semiquantitative grade 2 scale.
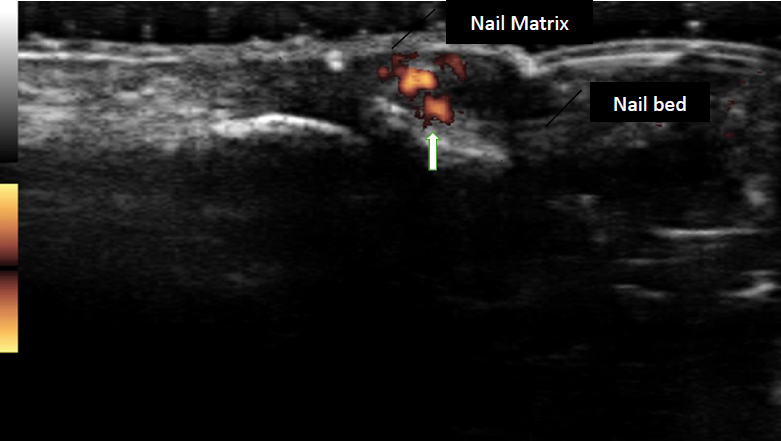
Ultrasound of the nail bed in a patient from group 3. Arrow indicates flow capture with power doppler, semiquantitative grade 2 scale.
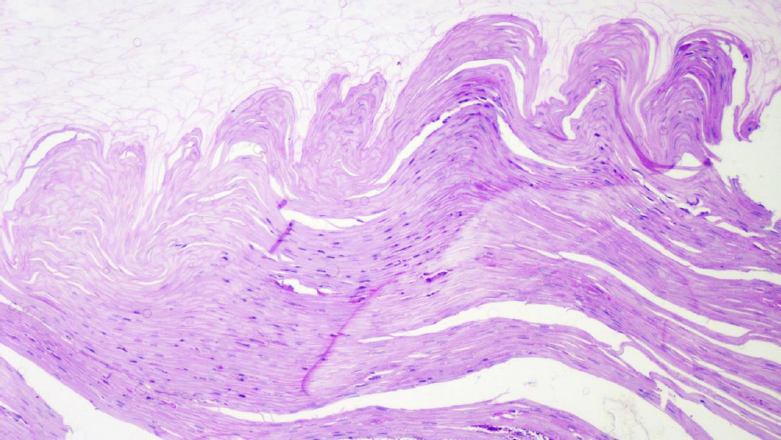
Photomicrograph of nail clipping from patient with onychodystrophy and cutaneous psoriasis. The nail transition zone between the nail plate (upper) and subungual region (lower) is clear. Accentuated hyperkeratosis and keratosis are visible in the subungual region, with the presence of some neutrophils. H&E staining, 20x objective lens.
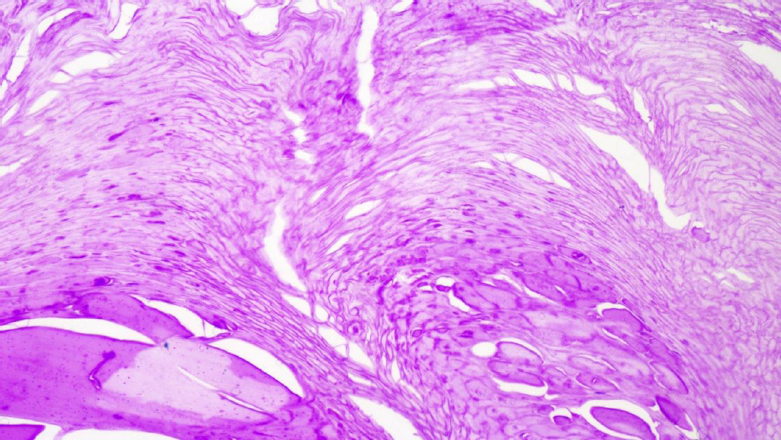
Photomicrograph of nail clipping from patient with onychodystrophy and psoriatic arthritis. The nail transition zone is blurred, and the transition between the nail plate (upper) and the subungual region (lower) cannot be clearly seen. In the subungual region, note predominant hyperkeratosis and parakeratosis with serous lakes. H&E staining, 20x objective lens.
| Group 2 (n=30) | Group 4 (n=30) | p | |
|---|---|---|---|
| Neutrophils (%) | 18.64% | 12.73% | 0.39 |
| Serous lakes | 37.29% | 29.09% | 0.35 |
| Parakeratosis | 52.54% | 47.27% | 0.53 |
| Blurred nail transition zone | 27.12% | 25.45% | 0.84 |
| Width of nail plate | 0.85 | 0.91 | 0.31 |
| Width of subungual plate | 0.48 | 0.44 | 0.24 |
3.3. Correlation between Ultrasound and Microscopic Variables
Microscopic thickness of the nail plate demonstrated a significant correlation with both grayscale score for the nail plate (p=0.002) and nail bed thickness (p=0.012). Additionally, the presence of neutrophils in the microscopic analysis was associated with increases in nail bed thickness (p=0.005) and grayscale score for the nail plate (p=0.00001). Serous lakes were found to be significantly associated with average nail bed thickness (p=0.013) and power doppler activity in the nail bed (p=0.009). The presence of blood also demonstrated a significant correlation with higher average grayscale values for the nail plate (p=0.005). Finally, blurring of the nail transition zone was significantly associated with mean nail bed thickness (p=0.001) and increased average colored doppler activity in the nail bed (p=0.018) (Table 2).
4. DISCUSSION
Ultrasound and nail clipping are increasingly used in dermatology to evaluate nail psoriasis. The most common ultrasound parameters used in this assessment include nail bed thickness, loss of definition, structural alterations in the nail plate, and changes in vascularization. While ultrasound maintained consistency between abnormalities in grayscale and in power Doppler and the severity of onychodystrophy, it has not proved useful for differentiating patients with and without arthritis [16-18]. Similarly, even though nail clipping is a diagnostic method used in nail psoriasis, it also cannot differentiate patients with and without psoriatic arthritis [3, 7, 15].
The progression of cutaneous psoriasis to psoriatic arthritis (PA) is a topic of great interest in dermatology as well as rheumatology. Various prognostic factors, such as the presence of onychodystrophy and the severity of cutaneous psoriasis, have been investigated as potential indicators of risk for developing PA. In this present study, we observed that onychodystrophy was more related to psoriasis severity indexes such as PASI and BSA than the presence of arthritis. This relationship suggests that onychodystrophy may better reflect the severity of psoriasis as a whole rather than serve as a specific marker of arthritis. Some studies suggest that genetic factors, obesity and arthralgia may indicate an increased risk of progression to PA [19, 20].
| Groups 2 + 4 | |||
|---|---|---|---|
| Neutrophils (%) | Present (n=17) | Absent (n=121) | p |
| Thickness of nail bed | 3.78 mm | 3.24 mm | 0.005 |
| GS nail plate | 4.29 degrees | 1.55 degrees | 0.00001 |
| Serous lakes | Present (n=56) | Absent (n=83) | p |
| Thickness of nail bed | 3.51 mm | 3.15 mm | 0.013 |
| PD nail bed | 1.79 points | 1.18 points | 0.009 |
| Blood | Present (n=12) | Absent (n=126) | p |
| GS nail plate | 3.42 degrees | 1.74 degrees | 0.005 |
| Blurred nail transition zone | Present (n=43) | Absent (n=95) | p |
| GS nail plate | 2.60 degrees | 1.56 degrees | 0.001 |
| PD nail bed | 1.93 points | 1.21 points | 0.018 |
The presence of neutrophils in nail clippings was significantly associated with a higher average PASI score (p=0.032), greater mean BSA value (p=0.032), and higher NAPSI score (p=0.008). However, it had not yet been described to what extent the presence of these neutrophils was correlated with ultrasound findings in nail psoriasis. In this present study, the presence of neutrophils was significantly associated with a higher average grayscale score for the nail plate (p=0.00001) and greater perfusion activity in the nail bed shown via Doppler (p=0.039).
Attention has recently returned to the role played by neutrophil extracellular traps (NETs) in psoriasis since activated neutrophils that produce NETs are abundant in cutaneous psoriatic plaques, pustules, and the blood serum of patients with psoriasis. The findings of this present study, especially the correlation between the presence of neutrophils in nail clippings and ultrasound alterations, highlight the importance of these cells in the pathogenesis of psoriasis and psoriatic arthritis. Recent studies suggest that neutrophils, by forming NETs, play a crucial role in the chronic inflammation of psoriasis [21]. The NETs activate the production of IL-17, a key cytokine in mediation of the inflammatory response in psoriatic arthritis. This pathway, independent of IL-23, suggests new therapeutic targets for the treatment of PA that focus on inhibiting the formation of NETs or neutralizing the activity of IL-17. Biological therapies that block IL-17, like the binding inhibitors secukinumab and ixekizumab, have already proven effective in controlling inflammation and reducing cutaneous and articular lesions, indicating the potential of these approaches in managing patients with nail psoriasis and PA [22].
On the other hand, in line with the findings of Fonseca [7], we did not find a relationship between the presence of neutrophils in nail clippings and the presence or absence of arthritis. These findings raise the question of whether the relationship between PA and nail psoriasis could be exclusively attributed to a biomechanical/anatomical connection between the two conditions [23-26]. This interpretation could be plausible when psoriatic plaques appear on the hands and/or fingers simultaneously with onychodystrophy and disease in the finger joints. This present study, like the work of Fonseca,7 shows that the severity of onychodystrophy is more related to PASI, BSA and NAPSI values than the presence of arthritis. Furthermore, the greater prevalence of onychodystrophy observed in patients with PA 25,26 could reflect more careful attention given to examinations in these patients since they are monitored more frequently and in more detail due to their systemic condition. This hypothesis is reinforced by the possibility that patients who have psoriasis without arthritis may not undergo such detailed evaluations, resulting in an underdiagnosis of nail alterations. Observational studies that longitudinally follow the progression of nail alterations in patients with different degrees of clinical monitoring could clarify this question. Studies correlating the presence or absence of neutrophils in nail clippings with enthesitis or arthritis in the phalanges confirmed by ultrasound would also be interesting to better explore this hypothesis.
In this study, we demonstrated that structural alterations appearing in nail ultrasound exams are reflected in microscopic analysis. Besides the aforementioned presence of neutrophils, a significant correlation was found between the thickness of the subungual region of the nail in microscopy and in power Doppler on ultrasound (p=0.0004). Serous lakes were also significantly associated with mean nail bed thickness (p=0.013) and increased power Doppler activity in the nail bed (p=0.009).
One characteristic of dystrophic nails in patients with psoriasis is an irregular transition between the nail plate and the subungual regions seen via microscopy, as previously described by Werner et al. [15]. In our study, this microscopic irregularity was significantly associated with a higher average mean grayscale score for the nail plate (p=0.001) and greater perfusion in the nail bed shown by Doppler (p=0.018); this is the first report of this correlation in the literature.
One of the limitations of this study was the fact that all the ultrasounds were conducted by the same examiner, which could introduce interpretation bias. Future studies should include multiple examiners, ideally conducting blind evaluations to minimize the risk of interpersonal bias. Furthermore, the patients included in the study were receiving clinical treatment, which could have influenced the ultrasound and microscopy findings. The use of systemic therapies for psoriasis and PA (such as immunosuppressors and biologics) could alter the characteristics of nail and joint lesions, and controlled studies involving patients who are not receiving treatment could provide a clearer vision of the natural progression of these alterations. An untreated control group or the inclusion of a group receiving different types of treatment could better distinguish the effects of therapy on the alterations observed.
CONCLUSION
This is the first study in the medical literature that correlates clinical characteristics, findings from nail clippings, and alterations in nail ultrasound. The presence of neutrophils and serious lakes, increased thickness of the subungual region, and decreased sharpness of the nail transition zone in microscopy were significantly associated with specific alterations in grayscale and/or perfusion doppler of the nail bed. However, no microscopic or ecographic variables were found to be significantly associated with psoriatic arthritis. Additional studies are necessary to evaluate whether these alterations continue over time in patients with different stages of the disease or who are treated with different types of therapies.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: study conception and design: ACBB; data analysis and interpretation: BS; draft manuscript: AAT, TLS, BW. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DIPS | = Distal interphalangeal joints |
| PASI | = Psoriasis Area and Severity Index |
| NAPSI | = Nail Psoriasis Severity Index |
| GS | = Grayscale |
| PD | = Power Doppler |
| DIP | = Distal interphalangeal |
| MHz | = Megahertz |
| BSA | = Body surface area |
| PA | = Psoriatic arthritis |
| NETs | = Neutrophil extracellular traps |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research project was submitted to the Ethics Committee of the Mackenzie Evangelical Faculty of Paraná (CAAE: 36864720.4.0000.0103), Brazil and received a favorable opinion for the study to proceed under protocol 4.279.067 on September 15, 2020.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants involved in this study were thoroughly informed about ethical matters. They carefully reviewed the free and informed consent form and provided their signature as an agreement to participate.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author [A.A.T] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.